Runners and athletes, listen up! Iliotibial band syndrome is a common injury that can stop your training. It happens when the iliotibial band, a thick tissue on the outer thigh, gets inflamed. In Thailand’s active fitness scene, many people face this issue.
This injury often comes from too much use, especially in runners who run a lot. Bad form, uneven ground, and muscle imbalances can also cause it. But, there’s good news: you can fight ITB band syndrome with the right steps.
In this article, we’ll look at why this injury happens and how to treat it. We’ll talk about rest, stretching, and exercises to help you recover. Let’s get started and keep your IT band healthy!

Key Takeaways
- Iliotibial band syndrome is a common overuse injury in runners
- Symptoms include outer knee pain, especially during running
- Causes range from overtraining to biomechanical issues
- Rest and proper stretching are crucial for recovery
- Strengthening exercises can help prevent future flare-ups
- Gradual return to activity is key for successful rehabilitation
Understanding ITB Band Syndrome
ITB band syndrome is a common injury that affects the outside of the knee. It happens when the iliotibial band, a thick tissue from the hip to the shin, gets inflamed. This is due to repeated friction against the thighbone.
Definition and Overview
The iliotibial band helps stabilize the knee during movement. When it gets irritated, it can cause sharp pain on the outside of the knee. This pain usually gets worse with activity and better with rest.
Prevalence in Athletes
ITB band syndrome is common among runners, cyclists, and hikers. Activities that repeat a lot increase the risk. Studies show up to 12% of runners may get ITB band syndrome at some point.
| Sport | Prevalence Rate |
|---|---|
| Running | 12% |
| Cycling | 15% |
| Hiking | 8% |
Impact on Daily Activities
ITB band syndrome isn’t just for athletes. It can also affect daily life. Walking, climbing stairs, or sitting for long times can hurt. Knowing about the iliotibial band’s anatomy is key for treatment and prevention.
“ITB band syndrome can significantly impact an athlete’s performance and quality of life. Early recognition and proper management are key to a successful recovery.” – Dr. Jane Smith, Sports Medicine Specialist
Anatomy of the Iliotibial Band
The iliotibial band is a vital part of our body. It’s a thick, fibrous tissue on the outer thigh. It starts at the hip and goes down to the knee.
This band helps stabilize both the hip and knee joints. Its unique shape makes it crucial for movement.
At the top, it connects with two hip muscles: the tensor fasciae latae and the gluteus maximus. These connections make it strong. They help it move the hip.
As it goes down the thigh, it attaches to the femur (thighbone). This connection is through fibrous tissues.
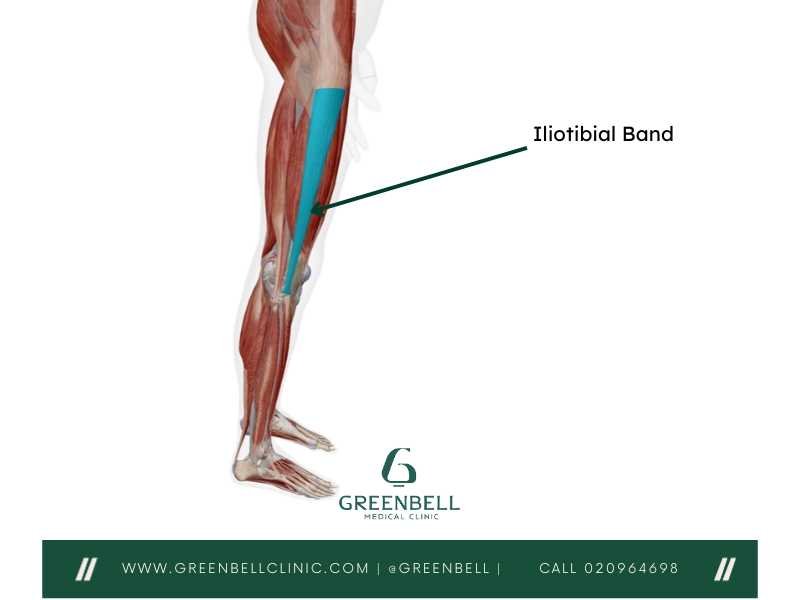
Near the knee, things get more complex. The iliotibial band splits into two parts:
- One part attaches to the lateral epicondyle of the femur
- The other part connects to the tibia (shinbone)
This split helps stabilize the knee during activities like walking and running. It works with other muscles and ligaments. Together, they control knee movement and prevent too much rotation.
Knowing how the iliotibial band works is important. It’s both a stabilizer and a facilitator of movement. This makes it a key part of our lower limbs’ mechanics.
Common Causes of ITB Band Syndrome
ITB band syndrome comes from several sources. Knowing these helps in stopping it before it starts. Let’s look at the main reasons for this painful issue.
Overuse and Repetitive Stress
Overusing your muscles is a big reason for ITB band syndrome. Runners and cyclists often face this problem. The constant rubbing of the ITB against the knee causes inflammation and pain.
Biomechanical Issues
Your body’s shape also matters. Problems like flat feet or uneven legs can stress the ITB. These issues change how you walk, making the band rub more.
Muscle Imbalances
Weak hip muscles are another risk. If your hips are not strong, your ITB has to work harder. This extra effort can irritate the band and cause pain.
By tackling these common causes, you can lower your risk of ITB band syndrome. Proper training and regular strength exercises are crucial for prevention.
Risk Factors for Developing ITB Band Syndrome
ITB band syndrome is common among runners. Knowing the risk factors can help prevent it. Let’s look at the main factors that increase a runner’s risk.
Running on uneven surfaces can stress the iliotibial band. This includes roads or trails with slopes. Wearing the right shoes is also key. Shoes that are too worn or don’t support well can cause problems.
Training mistakes can also lead to ITB band syndrome. Sudden increases in running or intensity can be too much. Running with poor form, especially if you adduct your hips too much, can strain the IT band. Weak hip muscles can also contribute to the issue.
| Risk Factor | Impact on Runners | Prevention Strategy |
|---|---|---|
| Uneven Surfaces | Increases stress on IT band | Vary running routes, avoid excessive hill training |
| Improper Footwear | Causes biomechanical issues | Replace shoes regularly, use appropriate support |
| Training Errors | Overloads IT band | Gradual mileage increase, proper form training |
| Muscle Imbalances | Strains IT band | Strengthen hip abductors, focus on core stability |
Leg length differences or excessive pronation can also increase risk. Past injuries to the knee or hip can change how you run. This can put more strain on the IT band. By tackling these risk factors, runners can lower their chances of getting ITB syndrome.
Symptoms and Signs of ITB Band Syndrome
It’s important to know the signs of ITB band syndrome early. This helps in managing pain better. The condition shows up in different ways, affecting how we move and perform in sports.
Pain Patterns and Locations
The main symptom is a sharp, burning pain on the outer knee. This pain gets worse during running or cycling, especially downhill. Some people also hear a clicking or popping sound as the band moves.
Associated Symptoms
People with ITB band syndrome might also feel:
- Stiffness or tightness on the outer thigh
- Swelling around the knee
- Warmth or redness at the pain site
- Difficulty walking or climbing stairs

Progression of Symptoms
If not treated, ITB band syndrome can get worse. At first, pain might only happen after long workouts. But as it gets worse, pain can start sooner and last longer.
In severe cases, pain can even be there when you’re not active. This can really affect your daily life. So, getting a diagnosis and finding ways to manage pain is crucial.
Diagnosis of ITB Band Syndrome
Diagnosing ITB band syndrome involves several steps. First, your doctor will ask about your activities and pain. They want to know about any changes in your exercise routine.
Next, a physical exam is done. The doctor will check for tenderness on your outer thigh and knee. They might also test your flexibility and strength to find the problem’s location and severity.
At times, imaging studies are needed. X-rays can help rule out other knee issues. MRI scans give a detailed look at soft tissues, confirming the diagnosis.
It’s important to rule out other conditions. Symptoms of ITB band syndrome can look like knee osteoarthritis or meniscus tears. Your doctor will look at all possibilities during the exam.
Getting a correct diagnosis is crucial for treatment. If you think you have ITB band syndrome, see a doctor right away.
Physical Examination Techniques
Doctors use specific tests to check for ITB band syndrome. These tests help pinpoint the problem and guide treatment plans. Let’s explore three key tests used in diagnosing this condition.
Renne Test
The Renne test checks for pain in the outer knee. The patient stands on the affected leg and bends it slightly. Pain on the outside of the knee suggests ITB band syndrome. This test is quick and easy to perform in a doctor’s office.
Noble’s Test
Noble’s test focuses on finding tender spots along the ITB. The patient lies on their back with their knee bent. The doctor applies pressure to the outer knee while straightening the leg. Sharp pain indicates a positive result for ITB band syndrome.
Ober’s Test
Ober’s test measures ITB tightness. The patient lies on their side with the affected leg on top. The doctor moves the top leg backward and lets it drop. If the leg doesn’t fall freely, it may signal a tight ITB.
| Test | Position | Action | Positive Sign |
|---|---|---|---|
| Renne Test | Standing | Bend affected leg | Outer knee pain |
| Noble’s Test | Lying on back | Straighten leg with pressure | Sharp pain |
| Ober’s Test | Side-lying | Drop top leg backward | Leg doesn’t fall freely |
These tests help doctors diagnose ITB band syndrome accurately. They’re simple yet effective tools in the hands of skilled healthcare providers.
Imaging Studies for ITB Band Syndrome
Imaging studies are key in diagnosing ITB band syndrome. A physical check-up is often enough. But, sometimes, more advanced tests are needed to confirm the diagnosis or rule out other issues.
X-rays are not usually used for ITB band syndrome. They can’t show soft tissues like the iliotibial band. Doctors might use X-rays to look for bone problems that could cause similar symptoms.
MRI scans give detailed views of soft tissues. They can spot inflammation around the IT band and any structural problems. MRI is especially helpful when symptoms don’t go away with simple treatments.
Ultrasound is a good, non-invasive choice for looking at the IT band. It lets you see the tissue in real-time and can find swelling or thickening. It also helps guide precise corticosteroid injections if needed.

| Imaging Type | Uses in ITB Band Syndrome | Advantages |
|---|---|---|
| X-ray | Rule out bone-related issues | Quick, inexpensive |
| MRI | Detailed soft tissue imaging | High-resolution images, detects inflammation |
| Ultrasound | Real-time tissue examination | Cost-effective, guides injections |
Imaging studies can offer important insights, but they’re not always needed. A detailed physical exam and a patient’s history are often enough. Imaging is usually used for more complex cases or when simple treatments don’t work.
Conservative Treatment Options
When dealing with ITB band syndrome, conservative treatments are often the first line of defense. These approaches aim to relieve pain and promote healing without invasive procedures.
Rest and Activity Modification
Resting the affected area is crucial for recovery. This means taking a break from activities that trigger pain. For runners, switching to low-impact exercises like swimming or cycling can help maintain fitness while allowing the ITB to heal.
Physical Therapy Exercises
Targeted exercises play a key role in rehabilitation. Strengthening the hip abductors and stretching tight muscles can improve biomechanics and reduce stress on the ITB. A physical therapist can design a personalized exercise program to address specific weaknesses and imbalances.
Pain Management Techniques
Effective pain management is essential for comfort and healing. Ice therapy can help reduce inflammation, especially after activity. Over-the-counter anti-inflammatory medications may provide relief, but should be used under medical guidance. Foam rolling and massage can also help alleviate tension in the ITB and surrounding tissues.
Combining these conservative approaches often yields the best results. Patience is key, as recovery can take several weeks to months. Gradually returning to normal activities while maintaining a balanced exercise routine can help prevent future flare-ups.
Advanced Treatment Modalities
When simple treatments don’t work, doctors might suggest more advanced options for ITB band syndrome. These methods aim to tackle ongoing pain and swelling.
Corticosteroid injections are one such method. A doctor injects a strong anti-inflammatory into the affected area. This can quickly cut down pain and swelling, making it easier to move.
Extracorporeal shockwave therapy is another advanced choice. It uses sound waves to help heal the damaged tissue. Many people see a big drop in pain after a few treatments.
In rare cases, surgery might be needed. This involves either releasing or lengthening the iliotibial band to lessen friction. Doctors usually turn to surgery only after trying other treatments.

It’s key to remember that these advanced treatments are not the first choice. Doctors usually suggest them only when simpler methods don’t work well. Every person’s case is different, and the best treatment depends on their unique situation and medical history.
| Treatment | Duration | Recovery Time |
|---|---|---|
| Corticosteroid Injection | One-time procedure | 1-2 days |
| Shockwave Therapy | 3-5 sessions | No downtime |
| Surgery | 1-2 hours | 4-6 weeks |
Prevention Strategies for ITB Band Syndrome
Preventing ITB band syndrome is key for athletes and active people. By using the right techniques and habits, you can lower your risk of this painful issue.
Proper Training Techniques
Slowly increase your training to prevent injuries. Don’t boost your mileage or intensity by more than 10% each week. This helps your body adjust and lowers injury risks.
Strength and Flexibility Exercises
Adding specific exercises to your routine can help avoid ITB band syndrome. Work on strengthening your hip abductors, glutes, and core. Also, stretch the IT band and nearby muscles regularly.
- Hip abductor exercises: Side-lying leg lifts, clamshells
- Glute exercises: Bridges, squats, lunges
- Core exercises: Planks, Russian twists
- IT band stretches: Standing IT band stretch, foam rolling
Equipment Considerations
Choosing the right gear is important for prevention. Make sure your shoes fit your foot type and running style. Replace them every 300-500 miles to keep support at its best.
| Foot Type | Recommended Shoe Type |
|---|---|
| High arches | Neutral cushioned shoes |
| Normal arches | Stability shoes |
| Flat feet | Motion control shoes |
By using these prevention tips, you can lower your risk of ITB band syndrome. This way, you can enjoy your workouts more without worrying about injuries.
Conclusion
ITB band syndrome can be a real pain for athletes and active individuals. Early diagnosis and proper treatment are key to getting back on your feet. If you’re experiencing outer knee pain, don’t ignore it. Seek help from a medical professional to determine if you’re dealing with ITB band syndrome.
There are many treatment options available. From rest and activity changes to physical therapy exercises, you have choices. In some cases, advanced treatments might be needed. The goal is to find the right approach for your specific situation.
Prevention is just as important as treatment. By using proper training techniques and focusing on strength and flexibility, you can reduce your risk of developing ITB band syndrome. Take care of your body, listen to its signals, and enjoy your active lifestyle without the burden of this common condition.