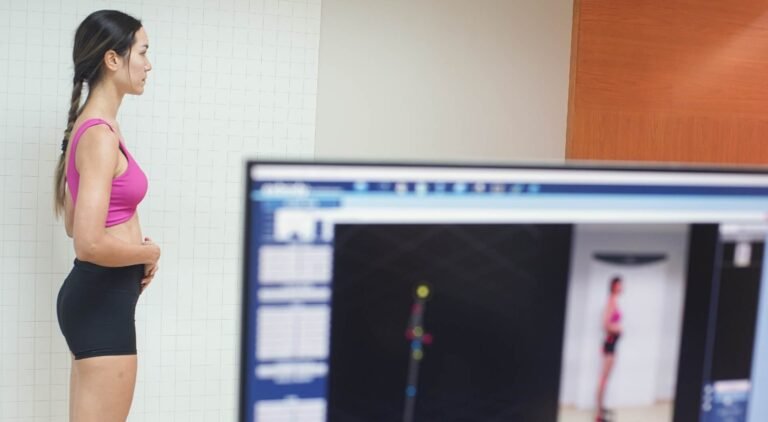
Managing the challenges of Stress Urinary Incontinence (SUI) can be a daily struggle impacting your confidence and quality of life. Greenbell Clinic offers specialized treatment to address SUI with a focus on providing tailored and effective solutions for women. Our SUI treatment is designed as a personalized strategy, meticulously identifying the factors contributing to your involuntary leakage during specific activities.
The dedicated experts at Greenbell Clinic utilize gentle methods that act as a targeted approach for the affected area, addressing the root cause of stress urinary incontinence. Whether your SUI is associated with muscle weakness, childbirth, or other factors, our approach aims to restore control and improve your overall comfort. Visit Greenbell Clinic today and embark on a journey to say goodbye to stress urinary incontinence, welcoming back confidence and a more active and carefree lifestyle. Our team is committed to providing the care and attention you need for a swift and effective recovery.
What is Women’s Health?
Women’s health pain refers to discomfort, pain, or medical conditions that specifically affect the female reproductive system or conditions that may disproportionately impact women. These issues can encompass a broad range of conditions and causations.
Greenbell Medical Clinic prioritizes women’s health, offering physical therapy and evidence-based interventions. Our approach empowers women to achieve optimal physical well-being through every stage of life.
Understanding the Condition
- Prevalence: Women’s health concerns are prevalent across different age groups, with specific issues such as pelvic floor dysfunction affecting a significant portion of the female population.
- Signs and Symptoms: Symptoms vary widely and can include pelvic pain, back pain during pregnancy, and musculoskeletal issues related to hormonal changes. Addressing these concerns is crucial for overall well-being.
- Complication: Untreated women’s health issues can lead to persistent discomfort, challenges during pregnancy and childbirth, and potential long-term complications affecting pelvic health.
Etiology and Risk Factors
- Menstrual Cramps (Dysmenorrhea): Pain associated with menstruation, often due to uterine contractions.
- Endometriosis: A condition where tissue similar to the lining of the uterus grows outside the uterus, causing pain, inflammation, and sometimes infertility.
- Pelvic Inflammatory Disease (PID): Infection of the female reproductive organs, often caused by sexually transmitted infections, leading to pelvic pain.
- Ovarian Cysts: Fluid-filled sacs that can form on the ovaries, sometimes causing pain and discomfort.
- Fibroids: Noncancerous growths in the uterus that can cause pain, heavy menstrual bleeding, and pressure on surrounding organs.
- Pelvic Floor Disorders: Conditions such as pelvic organ prolapse or urinary incontinence, which can cause pelvic pain and discomfort.
- Interstitial Cystitis: A chronic condition causing bladder pain and discomfort.
- Dyspareunia: Painful intercourse, which can be due to various factors such as infections, hormonal changes, or psychological factors.
- Vulvodynia: Chronic pain or discomfort in the vulva area without an identifiable cause.
- Menstrual Disorders: Conditions like menorrhagia (heavy menstrual bleeding) or oligomenorrhea (infrequent menstrual periods) that can cause pain and disrupt normal menstrual cycles.
- Menopausal Symptoms: Hormonal changes during menopause can lead to symptoms such as hot flashes, mood changes, and discomfort.
- Breast Pain: Conditions like mastalgia or fibrocystic breasts can cause breast pain.
- Polycystic Ovary Syndrome (PCOS): A hormonal disorder that can cause pain, irregular periods, and ovarian cysts.
- Pregnancy-related Pain: Conditions such as round ligament pain, back pain, or pelvic pain during pregnancy.
- Reproductive Organ Cancers: Conditions such as ovarian cancer, uterine cancer, or cervical cancer can cause pain in the pelvic region.
- Chronic Pelvic Pain Syndrome: Long-term pelvic pain without an apparent cause, often affecting the lower abdomen.
Service and Treatment
We are dedicated to providing care through evidence-based interventions. Whether it’s addressing the unique challenges of pregnancy-related discomfort or focusing on pelvic floor issues, our physiotherapists are committed to empowering women on their journey to attain optimal physical well-being. Through personalized and comprehensive approaches, we strive to enhance the quality of life for women, ensuring that they receive the highest standard of care tailored to their specific needs.
FAQ
What is women’s health physiotherapy, and what conditions does it address?
Women’s health physiotherapy focuses on conditions specific to women, including pelvic floor dysfunction, prenatal and postnatal care, urinary incontinence, and musculoskeletal issues related to pregnancy and childbirth.
Can physiotherapy help with pelvic floor issues, and what techniques are used?
Yes, physiotherapy is effective for pelvic floor issues. Techniques include pelvic floor exercises, biofeedback, and manual therapy to improve strength, coordination, and function.
Is physiotherapy beneficial during pregnancy, and what issues can it address?
Yes, physiotherapy is beneficial during pregnancy. It can address issues such as back pain, pelvic girdle pain, postural changes, and preparation for labor through exercises and education.
Can physiotherapy help with postpartum recovery, and when should it be initiated?
Physiotherapy is valuable for postpartum recovery. It can be initiated as early as a few weeks after childbirth, addressing issues like pelvic floor weakness, abdominal separation, and regaining overall strength.
How does physiotherapy address urinary incontinence in women?
Physiotherapy for urinary incontinence involves pelvic floor exercises, bladder training, and lifestyle modifications to improve bladder control and reduce leakage.
Can physiotherapy help with conditions like endometriosis or painful intercourse?
Yes, physiotherapy can assist in managing conditions like endometriosis and painful intercourse through techniques such as pelvic floor relaxation, manual therapy, and exercise programs tailored to specific needs.
Is there a role for physiotherapy in managing menopausal symptoms?
Yes, physiotherapy can play a role in managing menopausal symptoms, addressing issues like bone health, joint pain, and maintaining overall physical well-being through exercise and lifestyle recommendations.
Can physiotherapy help with premenstrual syndrome (PMS) symptoms?
Physiotherapy can offer relief for certain PMS symptoms through exercise, relaxation techniques, and addressing musculoskeletal discomfort associated with the menstrual cycle.
How can physiotherapy assist women with breast cancer recovery?
Physiotherapy plays a vital role in breast cancer recovery, addressing issues such as post-surgery mobility, lymphedema management, and overall rehabilitation to enhance quality of life.
Are there specific exercises for women’s health that can be done at home?
Yes, physiotherapists often provide home exercise programs tailored to women’s health needs. These may include pelvic floor exercises, core strengthening, and stretches to address specific conditions and promote overall well-being.